Aspects
PTCA, or percutaneous transluminal coronary angioplasty, is a minimally invasive procedure that opens blocked coronary arteries to improve blood flow to the heart muscle.
Local anesthesia numbs the groin region first. A doctor then inserts a needle into the femoral artery, the artery that runs down the leg. Doctors insert a guidewire through the needle, remove the needle, and replace it with an introducer, an instrument with two ports for inserting flexible devices. A thinner guidewire replaces the original. A long, narrow tube called a diagnostic catheter is passed over the new wire, through the introducer, and into the artery. Afterward, it is guided to the aorta and the guidewire is removed.
A doctor injects dye into a coronary artery and takes an X-ray with the catheter at the opening.
When it reveals a treatable blockage, the doctor backs out the catheter and replaces it with a guiding catheter before removing the wire.
A thinner wire is inserted and guided across the blockage. A balloon catheter is then inserted. A balloon is inflated for a few seconds to compress the blockage against the artery wall. It is then deflated. To widen the passage, the doctor may inflate the balloon a few more times, each time filling it a little more.
Repeat this process at each blocked or narrowed site.
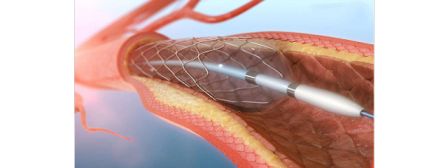
A stent, a latticed metal scaffold, may also be placed within the coronary artery to keep it open.
Following compression, dye is injected and an X-ray is taken to check for changes in the arteries.
The catheter is then removed and the procedure is complete.
The objectives are:
- Describe the indications for PTCA.
- Describe the contraindications to PTCA.
- Describe the complications of PTCA.
- To enhance the delivery of care for patients undergoing PTCA, it is important to improve care coordination among the interprofessional team.
Physiology and Anatomy:
Right and left coronary arteries supply the heart with blood. The left coronary artery (LCA) splits into the left anterior descending (LAD) and left circumflex artery (LCX) branches. LCA supplies blood to the left ventricle. The right coronary artery (RCA) is divided into the posterior descending artery (PDA) and a posterolateral branch (PL).
The RCA supplies blood to the ventricles, the right atrium, and the sinoatrial node. The myocardium is supplied with oxygen and nutrients by the coronary arteries, and their blockage can cause serious adverse health effects. In coronary artery disease, plaque builds up within the coronary arteries, narrowing and blocking the arteries, reducing blood flow to the myocardium.
Signs:
PTCA's indications depend on several factors. Those with stable angina symptoms who do not respond to maximal medical therapy will benefit from PCI. It provides relief from persistent angina symptoms despite maximal medical therapy. ST-elevation myocardial infarction (STEMI) resulting in 100% occlusion of the coronary artery is indicated for emergency PTCA.
STEMI patients are taken directly to the cath lab upon presentation to prevent further myocardial muscle damage. Patients with non-ST-elevation myocardial infarction (NSTEMI), or unstable angina (also known as acute coronary syndromes), are usually taken to the cardiac catheter lab within 24 to 48 hours.
Restrictions:
Contraindications to PTCA are limited. There is a risk of acute obstruction or spasm of the left main coronary artery during the procedure in patients with left main CAD. The procedure is also not recommended for patients with hemodynamically insignificant (less than 70%) stenosis of the coronary arteries.
Inventories:
Initially, PCI was performed solely with balloon catheters. As a result of subclinical outcomes and vessel re-stenosis, other devices such as atherectomy devices and coronary stents were introduced. The use of atherectomy devices alone resulted in poor outcomes. Due to improved clinical outcomes, coronary stents are the most widely used intracoronary devices in PTCA. Traditional bare-metal stents (BMS) and drug-eluting stents (DES) are two types of stents available. DES has a polymer coating that reduces inflammation and endothelial cell proliferation. The most recent DES used in the United States is sirolimus, everolimus, and zotarolimus. The use of antiplatelet therapy is important during the first 12 months after PTCA, to allow adequate endothelial cell formation over the metallic stent.
People
PTCA is performed by a team consisting of an interventional cardiologist, a nurse, and a radiology technologist. The team members must have specialized and extensive training in the procedure.
Planning:
A multidisciplinary team evaluates patients and performs pre-procedure testing to determine their suitability for the procedure. Inquiring about allergies to seafood or contrast agents in the past is vital. Pre-procedure laboratory tests include PT and PTT, serum electrolytes, BUN, and creatinine. Hydration is essential. If possible, anticoagulants should be ceased as part of the medication review. Also, common medications such as NSAIDs or ACEIs can be avoided to prevent worsening renal disease.
Before cardiac catheterization, the diabetes medication metformin is held to prevent worsening renal insufficiency and lactic acidosis. A six to eight-hour fast is recommended before the procedure. In cases involving radial artery access, patients are often given intra-arterial calcium channel blockers, nitroglycerin, and heparin to prevent vasospasm. To obtain informed consent, the health care provider should thoroughly explain the procedure and its risks to the patient.
Method:
Under local anesthesia, the procedure is performed. To avoid stress and calm the patient, conscious sedation is routinely administered. The most common approach is the percutaneous femoral (Judkins) approach. After the patient has been anesthetized with a superficial injection of lidocaine over the skin and subcutaneous tissue over the right femoral artery, a needle is inserted into the artery (percutaneous access).
Following the successful insertion of the needle, a guidewire is inserted through the needle into the blood vessel lumen. After the needle is removed, the guidewire remains in the vessel lumen. Over the guidewire, an introducer is placed into the femoral artery. Next, the guidewire and introducer are removed, leaving the sheath in the vessel lumen. This allows easy access to the femoral artery lumen. In the next step, a long narrow tube called a "diagnostic catheter" is advanced through the sheath with a long guidewire in the catheter lumen. Using the guidewire, the diagnostic catheter is passed retrograde through the femoral artery, iliac artery, descending aorta, and over the aortic arch to the proximal ascending aorta.
As the guidewire is removed, the tip of the diagnostic catheter is left in the ascending aorta. With a syringe, the diagnostic catheter is attached to a manifold. By using the manifold, it is possible to inject contrast, measure inter-arterial pressure, and administer medications.
A diagnostic catheter is then inserted into the ostium of the left main coronary artery or right coronary artery. Multiple cine angiography images of both arteries are obtained after contrast dye is injected. A PTCA may be performed if one of the arteries has severe stenosis. The diagnostic catheter is removed and replaced with a similar guide catheter. Guide catheters have a larger lumen diameter for easier passage of wires and balloons during angioplasty. Following placement of the guide catheter in the ostium of the respective artery, a PTCA guidewire is advanced through the catheter and across the stenosis.
Once the guidewire has been passed across the stenosis, it is left in place until the procedure is complete. Over the PTCA guidewire, a balloon wire can be placed and advanced until the balloon is directly over the stenosis. A cardiologist controls the direction and movement of the PTCA guidewire and balloon wire by twisting the part of the wire that sits outside the patient. After that, the balloon is inflated and deflated repeatedly until the artery is patent. Usually, a stent is needed. The balloon wire is removed and replaced with a stent.
Stents are latticed metal scaffolds that are crimped over balloons. The stenosis is then treated with the stent, which is then expanded by the balloon. After the stent is expanded, it cannot be removed from the artery. After the balloon is deflated, the stent remains in place. It can maintain patency over time. An artery is checked for patency by repeated injections of contrast media.
After insertion of the stent and expansion of the vessel, the balloon wire is The PTCA guidewire is then removed. Anticoagulation is administered to prevent clot formation during the procedure. Depending on the technical difficulties of the case, the entire process can take 30 minutes up to 3 hours.
Problems
Although there are risks associated with PTCA, major complications are rare. Angioplasty is associated with a 1.2% mortality rate. Older adults, people with kidney disease or diabetes, women, and those with massive heart disease are at a higher risk for complications. Likely complications include hematoma at the femoral artery insertion site, pseudoaneurysm of the femoral artery, infection of the skin upper femoral artery, embolism, stroke, kidney injury from reverse dye, hypersensitivity to dye, vessel rupture, coronary artery dissection, bleeding, vasospasm, thrombus formation, and acute MI. Restenosis of the stented vessel is a long-term risk.
Clinical Importance:
The procedure is performed under local anesthesia and is an alternative to coronary artery bypass surgery (CABG). As compared to CABG, PTCA has a lower rate of morbidity and mortality, shorter recovery time, and lower cost. In about 90% of patients, it improves blood flow through the coronary arteries, alleviates angina symptoms, and increases exercise capacity. Generally, it prevents arterial narrowing. Different modeling studies have presented different conclusions regarding the cost-effectiveness of PTCA and CABG in patients with myocardial ischemia that do not respond to medical therapy.
Improving the performance of healthcare teams:
PTCA is not an easy procedure, and despite the advances in technology, it comes with complications and risks. All patients should be informed about the procedure and its potential complications. To reduce the risk of recurrences and complications after surgery, it is important to maintain a healthy diet, exercise, and reduce stress. Patient-centered care is demonstrated by the heart team. The best solution for each patient is provided by experts from different fields of medicine.



Feel free to ask me any questions you might have